How the FlexCard Reloads
Qualifying allowances are loaded onto a reusable card.
Quarterly balance reloads on January 1, April 1, July 1, October 1.
Monthly balance reloads on the 1st of the month.
Balance does not carry over.
Start Using Your FlexCard
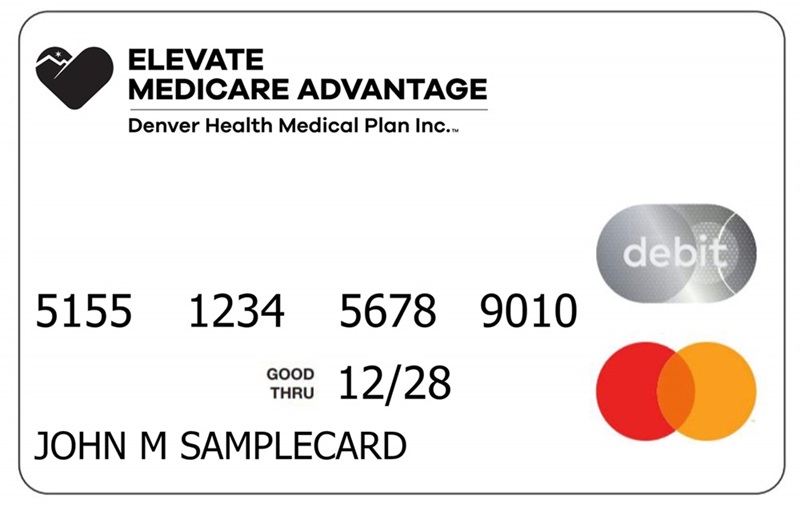
1. Get Your Pre-Activated FlexCard in the Mail
Existing or re-enrolling members should use their previous card, it will be re-activated upon your enrollment start date.
Pro Tip: To best protect your card allowance, you have the option to add a PIN number to secure your FlexCard by calling 303-602-2111, TTY 711 and selecting Option 2. Follow the prompts to add a PIN number to your FlexCard. Note: Costco requires a PIN for purchases.
2. Use Your FlexCard to Buy Eligible Items
Participating merchants include King Soopers, Safeway, Costco, Walmart, Target, Walgreens, CVS and Dollar General. You may also order eligible healthy food or OTC items from our catalog (for a printed catalog or to place an order, call 1-833-881-1423). Note: Walmart's approved product list is not available to DHMP or members, and some items approved in the FlexCard app may not be covered.
Pro Tip: Be sure to use your allowance before 6pm MT on the day the quarter or month ends. Transactions after 6pm may process the next day and deduct from the next quarter or month due to card processing rules.
3. Access the FlexCard Portal
You can access the FlexCard portal online, or download the Elevate Medicare FlexCard mobile app on your Android or iPhone.
4. Check Your Balance Anytime
Check your balance by logging into the FlexCard portal or by calling Health Plan Services and using the automated prompt at 303-602-2111, select option 2. Have your card ready, so you can enter the card number when prompted.
Elevate Medicare Advantage FlexCard FAQs
You can shop in-store at the following approved stores:
- Safeway
- King Soopers
- Costco
- Walmart
- CVS
- Target
- Walgreens
- Dollar General
To find an approved store nearby, download the Elevate Medicare FlexCard mobile app on your Android or iPhone.
- You can purchase items online at Walgreens.com and Medline in the FlexCard Portal.
- You can also place your order with Medline by phone or by mail by using the OTC/food catalog.
1-833-881-1423 (TTY 711)
Medline
PO Box 18522
Palatine, IL 60055
Call reach Medline by calling their Benefit Services at 1-833-881-1423 (TTY 711).
You can request an English-language catalog be mailed to you in the FlexCard Portal.
For a Spanish-language catalog by mail, submit your request to Medline here.
You can also request a catalog be mailed to you in either English or Spanish by calling Medline at 1-833-881-1423 (TTY 711).
The FlexCard mobile app will allow you to scan an item to confirm if it's eligible. Download the Elevate Medicare FlexCard mobile app with your Android or iPhone.
If you don't want to use the app, you can:
- Purchase items and qualifying items will automatically be covered with eligible FlexCard funds when you check out
- Place your order with Medline by phone or by mail using the OTC/food catalog.
Yes and you can check out all your items out at once. Once it is time to pay, you will swipe your Elevate Medicare FlexCard and the card will automatically pay for any eligible items up to your eligible allowance. The system will then ask you for another form of payment for any non-eligible items or items above the balance on your Elevate Medicare FlexCard.
No, you should swipe it like a regular MasterCard and it will pay for eligible items up to the balance on your card. After it has finished applying the funds, it will ask you for another form of payment for the remaining balance.
Transactions can take up to 7 business days to settle, if the store does not settle or reverse the transaction on the 8th business day the funds will be returned to your account.
No. If you re-enroll, a new card is not automatically reissued, unless you left the plan for greater than 90 days. If you left for less than 90 days and need a new card, call Health Plan Services at 303-602-2111, toll-free 1-877-956-2111 or TTY 711, 8 a.m. - 8 p.m., seven days a week.
A PIN can secure your card in case it is lost/stolen, so no one can utilize your eligible funds. To set up a PIN call 303-602-2111 and select option 2. Have your card ready to provide when prompted and utilize the automated prompts to set up a PIN.
If you try to purchase an item with your FlexCard that is declined, you may submit it for review. Simply fill out the FlexCard Declined Submission form. Failure to provide all requested information will result in no review of the declined transaction(s), due to not enough information to troubleshoot.
If you would like Elevate Medicare Advantage to consider adding a product to the APL, submit the FlexCard Declined Submission form with product information. Please allow 45 days for item to be considered for addition to the APL. This is not a guarantee the item will be added.
If you notice an unauthorized transaction, you will need to file a dispute using the Dispute Form located in your FlexCard member portal under Tools & Support. Have the date and amount of the transaction ready before completing the form. Once finished, send the form to the address provided on the document. If your dispute is approved, the FlexCard vendor will credit your account for the approved amount.
It depends on whether the refund is from the same plan year.
- Refunds and credits from disputes carry forward to future benefit periods within the plan year.
- Refunds and credits from disputes will continue to be available through the end of the plan year.
- Refunds and credits from disputes will not automatically roll over into the next plan year.
For additional security measures, the app or web portal may request multi-factor authentication. The system will send an additional password to your mobile phone or email on file in some scenarios like the first time you register for the portal or on a new device, if you request a new card, or if you change your password. If you need to update your phone number or email, please contact our Health Plan Services at 303-602-2111 (TTY 711) and talk to a representative.
The FlexCard should be used first because the EBT (SNAP) card may cover additional items. Or you can pull out items you know you are covered by the FlexCard and purchase those, then do a separate transaction using your EBT (SNAP) card.
*The Healthy Food Allowance offered with the Elevate Medicare Choice (HMO D-SNP) plan is part of special supplemental program for the chronically ill. Not all members qualify. Other eligibility and coverage criteria apply. Eligible conditions include cancer, chronic heart failure, diabetes, chronic lung disorders, and chronic and disabling mental health conditions. Other conditions also apply that are not listed.


