Online Prior Authorization Requests
Online Prior Authorization Requests for medical and behavioral care can be accessed through the secure Provider Portal. If you do not already have a DHMP Provider Portal account, please contact your local administrator to add you to your organization’s group account or if you are going to be your organization’s local administrator, please register now. For questions about provider portal registration, please email dhmp_portal@dhha.org.
Faxed Prior Authorization Requests
You may also fax Prior Authorization Requests to the following:
– Outpatient fax: 303-602-2128
– Inpatient Admit and Discharge Notification fax: 303-602-2127
– Inpatient Clinical Records fax: 303-602-2004
– Urgent/Expedited fax: 303-602-2160
For details regarding retrospective requests see Retrospective Requests (Post Service). Contact Health Plan Services if you have questions at 303-602-2140.
Early Intervention Requests
Submit Health Information Authorization (HIA) requests and Individualized Family Service Plan (IFSP) requests via the Early Intervention Request form. This form is ONLY for providers serving our CHP+, Exchange/CO Option and Denver Health Employer Plan members participating in Early Intervention Services.
Provider Resources
The Utilization (UM) Department at Denver Health Medical Plan, Inc. (DHMP) is designed to ensure the delivery of high quality and cost-efficient health care for our members. Services are intended to evaluate and promote high quality and cost-effective care for our insured members, including our large group plans, Medicare Advantage plans, Exchange/CO Option plans, CHP+ and Medicaid plans. We work to ensure that our members receive the right care, in the right setting, by the right provider.
Utilization Management Objectives:
UM Department aims to achieve the following for all members:
- To assure effective and efficient utilization of facilities and services through an ongoing monitoring and education program. The program is designed to identify patterns of over or under-utilization patterns and inefficient use of resources.
- To assure fair and consistent UM decision-making by using evidence-based, decision support criteria from guidelines such as MCG, Simplr and Denver Health Medical Plan, Inc. Medical Policies.
- To focus resources on a timely resolution of identified problems.
The Authorization Process
It’s important to understand the difference between a referral and an authorization – and how to obtain each one.
- A referral is the process of one provider, usually the Primary Care Provider (PCP), sending a patient to another provider (usually a specialist) for consultation or services. If a member needs to see a specialist, they should ask their Denver Health PCP for a referral. *
- An authorization is a process of reviewing requests for health services to make sure the service is both medically necessary and appropriate for the member. The review also determines whether or not the requested service is a covered benefit under the member’s benefit plan.
Please see the List of Services Requiring Prior Authorization on this page for the services that require prior authorization. The exception to this rule applies to the DHHA Point of Service (POS) members who choose to use their First Health Network option. They do not need an authorization to see providers in the First Health Network.
Authorization is required for all services provided outside of Denver Health networks Please refer to the member handbooks on this website for details.
Communication (Phone, Fax, Webform)
Members
Members should contact their physician to initiate an authorization.
Providers
DHMP Health Plan Services staff is available for UM issues during normal business hours, Monday through Friday, 8 a.m. to 5 p.m., excluding holidays. Providers may contact Utilization Management by fax to send authorization requests and clinical information. The DHMP Utilization Management Department can receive faxes seven days a week, including holidays. Please use the Prior Authorization Request Forms.
Contact by fax or phone:
- Outpatient fax | 303-602-2128
- Inpatient Admit and Discharge Notification fax | 303-602-2127
- Inpatient Clinical Records fax | 303-602-2004
- Urgent/Expedited fax | 303-602-2160
- Contact Health Plan Services by phone* | 303-602-2100
Phone calls will be returned within one business day.
Provider Participation Status Definitions
Provider Participation Status is identified and described as follows:
- Tier 1 Providers
Contracted providers considered in-network, listed in the Provider Directory, do not require authorization, unless service is included in the list of SERVICES REQUIRING PRIOR AUTHORIZATION.- NOTE: DHHA facilities and DHHA providers who perform services at DHHA do not require prior authorization for any services, with this exception: authorization required for outpatient therapy after the first 30 visits.
- Tier 2 Providers
Contracted Providers considered out-of-network, not listed in the Provider Directory, require prior authorization for all services. - Tier 3 Providers
Non-contracted, out-of-network providers for all lines of business, not listed in the Provider Directory, require prior authorization for all services and may require a One Time Agreement (OTA).
Provider tiering status may vary by plan.
Services must meet medical necessity and be a covered benefit, regardless of provider tiering status.
General Rules
- Urgent, emergency and observation care DO NOT require Prior Authorization.
- DHHA facilities and DHHA providers who perform services at DHHA do not require prior authorization for any services. **Exception – authorization required for outpatient therapy after the first 30 visits.
- Services not requiring prior authorization are subject to audit. If in an audit, services did not meet medical necessity, there will be a possibility of recoupment.
- Excluded services are not covered. Excluded services will be denied as a non–covered benefit, per the member’s Evidence of Coverage (EOC).
- Providers are responsible for verifying eligibility and benefits before providing services to all DHMP members. Prior Authorization is not a guarantee of payment for services. Payment is made in accordance with a determination of the member’s eligibility, benefit limitations/exclusions, evidence of medical necessity during the claim review and provider status with DHMP.
- Failure to obtain prior authorization before providing care for the services listed below may result in a denial for reimbursement.
- If a DHMP member is admitted to your facility, you must notify DHMP within 24 hours. If you fail to notify DHMP during this window of time, the member’s admission and continued stay may be denied for “untimely notification.”
- Services submitted after the start of care will be considered Retrospective Requests (post service).
- Retrospective authorization requests will be reviewed for medical necessity when:
- Request is less than < 15 calendar days post service.
- If request is greater than > 15 calendar days, provider must additionally provide rationale for late submission. For example, provider documents that they were unable to get insurance verification.
- Request is less than < 15 calendar days post service.
- Retrospective authorization requests will not be processed and will be returned with instructions to follow the Claims Reconsideration Process when:
- Claims have been submitted. If claims have already been submitted, please follow the instructions given by the Claims Department for denials received for not obtaining a prior authorization by DHMP prior to services being rendered.
- Request is greater than > 90 days post service
- Retrospective authorization requests will be reviewed for medical necessity when:
Resources
Providers can submit Prior Authorization Requests by either submitting an ONLINE Prior Authorization Request form or by completing and faxing a PDF Prior Authorization Request form. If using a PDF form, it should be faxed to DHMP. If you have questions, please contact Health Plan Services at 303-602-2100.
- Inpatient Request Fax: 303-602-2127
- Outpatient Request Fax: 303-602-2128
- Urgent/Expedited Request Fax: 303-602-2160
UM PRIOR AUTHORIZATION REQUEST FORM
Denver Health Medical Plan Secondary Payer and Authorizations
Denver Health Medical Plan (DHMP) does not typically require authorization when the secondary payer. However, if the requested service was denied by the primary insurance as not a covered benefit or benefits have been exhausted, an authorization may be requested.
Please submit clinical information with the primary insurances denial letter or limitation/exhaustion letter with the authorization request to the Utilization Management (UM) Department.
Note: Prior Authorization is not a guarantee of payment for services. Payment is made in accordance with a determination of the member’s eligibility, benefit limitations/exclusions, and evidence of medical necessity during the authorization review and provider status with DHMP at the time services are rendered.
Denver Health Medical Plan Secondary Payer and Claims
Submit claims to the secondary insurance once you have billed the primary insurance and received payment or Explanation of Remittance (EOR). DHMP will need the bill total, how much the primary insurance paid and why primary didn’t pay the remainder of the balance.
Please include the adjustments and categories for the remaining balance for a seamless secondary claim process.
Secondary coverage may only cover part or all the remaining costs or not pay any of the remaining costs. There are steps in place to ensure that both plan/coverages do not pay more than 100% of the bill based on contractual and benefit plan arrangements.
Provider Forms
Refer to provider resources for forms and general information. If you have questions, please contact Health Plan Services at 303-602-2100.
List of Services Requiring Prior Authorization
|
Care Type |
Details |
|
Acute Physical Rehabilitation |
All acute/inpatient requires prior authorization |
|
Experimental/Investigational Services |
All experimental/Investigational medical and surgical procedures, equipment and medications |
|
Behavioral Health Services |
NOTE: Medicare Tier 1 Providers do not require authorization for any Behavioral Health Services |
|
Durable Medical Equipment (DME) and Prosthetics Purchases over $1,000 (billed with modifier NU or UE) |
See list of DME codes below. |
|
Durable Medical Equipment (DME) Rental |
All DME Rentals regardless of dollar amount (billed with modifier RR) |
|
Disposable Goods |
Authorization required if beyond benefit limit |
|
Early Intervention Services |
Medicaid:
|
|
Enteral and Total Parenteral Nutrition |
All oral, tube feed or TPN requires prior authorization |
|
Genetic Testing |
Tier 1 Providers:
Tier 2 and Tier 3 Non-Participating Providers:
|
|
Home Health |
|
|
Infertility Treatment |
All infertility treatment |
|
Long Term Acute Care (LTAC) |
All LTAC admissions require prior authorization |
|
Outpatient Physical Therapy (PT), |
Tier 1 Providers:
|
|
The following surgeries when performed in an inpatient, outpatient or office location |
Providers are responsible for verifying eligibility and benefits before providing services to all DHMP members |
|
Skilled Nursing Facility (SNF) |
Tier 1 Providers:
|
|
Some Specialty Rx/Infusions (based on federal and state regulatory guidelines and/or benefit plan limitations) |
See Specialty Rx/Infusions table below |
|
Transplants |
Includes: Transplant Evaluations, Pre- and Post-Operative Services/Care |
*Based on Federal and State regulatory guidelines and/or benefit plan limitations. Exclusion, limitations and/or requirements may apply.
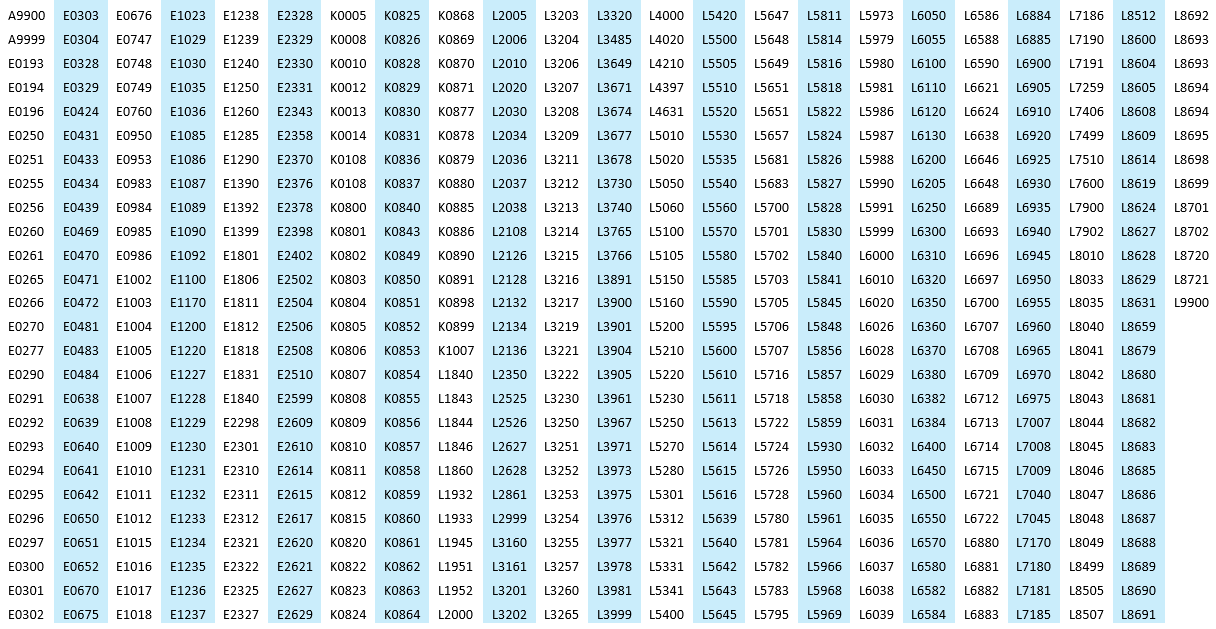
DME Codes
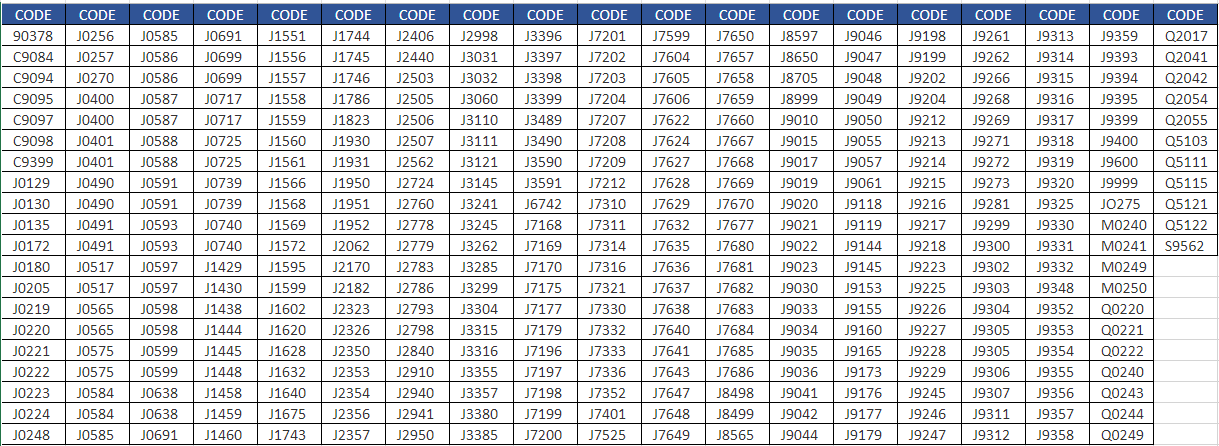
Specialty Rx/Infusions Requiring Prior Authorization
Regulatory Turnaround Time Requirements |
||||
| Type of Notification | Commercial Exchange and CO Option |
Commercial DHHA |
Medicaid and CHP+ |
Medicare |
| -Decisions- | ||||
| Urgent/ Concurrent |
72 Hours | 72 Hours | 72 Hours | 72 Hours |
| Expedited/ Urgent Preservice |
72 Hours | 72 Hours | 72 Hours | 72 Hours |
| Expedited Medical Drugs/ Part B Drugs |
72 Hours | 72 Hours | 72 Hours | 24 Hours |
| Standard/ Preservice |
15 Calendar Days | 15 Calendar Days | 7 Calendar Days | 7 Calendar Days |
| Standard Medical Drugs/ Part B Drugs |
15 Calendar Days | 15 Calendar Days | 7 Calendar Days | 72 Hours |
| Retrospective/ Postservice |
30 Calendar Days | 30 Calendar Days | 30 Calendar Days | 30 Calendar Days |
| -Extensions- | ||||
| Urgent/ Concurrent |
None | 48 Hours | 14 Calendar Days | 14 Calendar Days |
| Expedited/ Urgent Preservice |
48 Hours | 48 Hours | 14 Calendar Days | 14 Calendar Days |
| Standard/ Preservice |
15 Calendar Days | 15 Calendar Days | 14 Calendar Days | 14 Calendar Days |
| Retrospective/ Postservice |
15 Calendar Days | 15 Calendar Days | None | None |
| Part B Drug | NA | NA | NA | None |
Rationale:
- For all Commercial Lines of Business
Per NCQA 2025 Standard and Guidelines for the Accreditation of Health Plans, UM 5: Timeliness of UM Decisions have been changed from 24 hours to 72 hours for urgent concurrent admissions. - For Elevate Exchange Plans
Per NCQA 2025 Standards and Guidelines for the Accreditation of Health Plans, UM 5: Timeliness of UM Decisions, extensions are no longer allowed for urgent concurrent admissions.
Retrospective Requests (Post Service)
- Services submitted after the start of care will be considered retrospective requests.
- If claims have already been submitted, please follow the instructions given by the Claims Department for denials received for not obtaining a prior authorization by DHMP prior to services being rendered.
UM Process
Retrospective authorization request will not be processed when:
- Claims have been submitted
- Request is greater than > 90 days post service
Requests will be returned with instructions to follow the Claims Reconsideration Process.
Requests will be reviewed for medical necessity:
- When request is less than < 15 calendar days post service
- If request is greater than > 15 calendar days provider must additionally provide rationale for late submission. For example, provider documents that they were unable to get insurance verification.
- DHMP will not modify a request once a decision has been rendered.
- For any modification (extended dates or additional visits) to the original authorization request requires a new submission.
- Each submission must be on a new prior authorization form with a new cover sheet.
- Do not submit duplicate requests, as this will delay processing.
- Each prior authorization request submission will generate a new authorization number.
Internal Clinical Coverage Criteria
Denver Health Medical Plan (DHMP) has published internal clinical coverage criteria for the following services:
- Dental-Related General Anesthesia & Facility Charges
- Hair Prosthesis
- Oral/Enteral Feedings
- Positive Airway Pressure Device or Ventilator
Medicare Advantage Clinical Coverage Criteria
DHMP uses the Centers for Medicare and Medicaid Services (CMS) National Coverage Determinations (NCDs) and Local Coverage Determination (LCDs) criteria for services requiring authorization.
CMS Medical Necessity Coverage Requirements
Criteria Used for UM Decisions
Nationally accepted, evidenced-based clinical criteria sets are used when available. In cases in which the service is not addressed in any of the referenced criteria the clinical reviewers send to the DHMP medical director for guidance. UM staff will provide copies of the criteria to providers and members upon request.
- MCG Health™ Care Guidelines
- For the Medicare lines of business, National Coverage Criteria (NCD) and Local Coverage Criteria (LCD) criteria is used and is embedded within MCG Health Care Guidelines. In coverage situations where there is no NCD, LCD, or guidance in original Medicare Manuals, DHMP will defer to MCG or next available evidence-based criteria.
American Society of Addiction Medicine (ASAM) criteria is also embedded within MCG Health Care Guidelines. ASAM criteria is a multidimensional assessment that takes into account the patient's needs, obstacles and liabilities, as well as their strengths, assets, resources, and support structure. This information is used to determine the appropriate level of care across a continuum.
- Simplr
- This resource is useful in determining medical necessity for newer technology – criteria which are often not yet included in a national criteria set like MCG.
- UpToDate, Inc.
- A software system that is a point-of-care medical resource. The UpToDate system is an evidence-based clinical resource.
- Colorado Department of Health Care Policy & Financing (HCPF) Benefits Collaborative
- The Colorado HCPF Benefits Collaborative is a set of Benefit Coverage Standards that have been approved by the Colorado State Medicaid Director and are in effect for the Medicaid lines of business and product
- InterQual™
- Used only by Colorado Access (COA) for Medicaid Behavioral Health (BH) UM Reviews. BH Utilization Management has been delegated to COA by DHMP.
- Durable Medical Equipment (DME)
- MCG Health™ Care guidelines.
- HCPF Billing Manuals, Durable Medical Equipment, Prosthetics and Supplies (DMEPOS), DME HCPCS Codes.
- HCPF Portal – Fee Tables.
- Internal Coverage Criteria
- DHMP may establish coverage guidelines for services for which there are no clear evidence based clinical criteria.
- Member Handbook
- For all lines of business UM will review the Member Handbook for coverage determinations. The Member Handbook describes covered services based on member's plan, included and excluded coverage, and conditions for coverage.
General Guidelines
DHMP considers the member’s medical needs by using established health care guidelines based on medical evidence and state regulations to determine the appropriate frequency and/or quantity of the service(s) requested. The DHMP Physician Reviewer reviews all requests that do not meet these criteria
The coverage policies apply to the benefit plans administered by DHMP and may not be covered by all DHMP plans. Please refer to the member’s benefit document for specific coverage information. If there is a difference between this general information and the member’s benefit document, the member’s benefit document will be used to determine coverage. For example, a member’s benefit document may contain a specific exclusion related to a topic addressed in a coverage policy.
Coverage determinations for individual requests require consideration of:
- The terms of the applicable benefit document in effect on the date of service
- Any applicable laws and regulations
- Any relevant collateral source materials including coverage policies
- The specific facts of the request
Contact Health Plan Services to discuss plan benefits more specifically (303) 602-2100.
To easily locate an in-network provider for each plan, see Find a Provider at the top of this website.
- You can request a peer-to-peer review.
- A peer-to-peer (P2P) review is a telephone conversation between the physician reviewer who made the denial decision at the Plan and the requesting health care provider. This is an opportunity to discuss the denial without going through the formal appeal process.
- The request for a P2P review must be made within five (5) days of the determination notification by calling us at 303-602-2116. You will be asked to provide two options of availability. Note: Do not request same day availability, the physician reviewer needs at least a 24-hour notice to become available. Please include the time, date and phone number you can be reached.
- The physician reviewer will make two phone call attempts to make contact. If the outreach attempts are unsuccessful, additional dates will not be scheduled. If the five (5) day period has ended, you will need to file an appeal. Peer to peer reviews must occur between the ordering provider (or an alternative provider of equal licensing) and the physician reviewer. Office personnel or personnel that are not licensed to write an order for the requested services cannot conduct the call.
- You can file an appeal
- Filing an appeal is a formal review process controlled by state or national regulations. There are timely filing requirements and Personal Representative requirements.
- The denial letters clearly state all deadlines and requirements for filing an appeal. If you miss a deadline, you may no longer be able to appeal the decision.
- Providers can represent a Medicare Member without a signed Appointment of Representative Form (AOR) to designate the Personal Representative Status.
- All non-Medicare plans require a signed AOR form with both the member and representatives’ signature in order to file an appeal. Appeals will be pended and not processed if a signed AOR form is not received.
- How to file an appeal by plan coverage:
Child Health Plan Plus (CHP+)
Medicaid
Medicare
Exchange/Colorado Option
DHHA Employer Plans
When you need to refer a member to an in-network provider, see FIND A PROVIDER for access to the DHMP Provider Directory. You will need to know the member plan name. You can search by provider name, specialty, and/or location.
- With the exception of urgent/emergency care, any care given outside of the Plan service area will require prior authorization. The request must be reviewed for medical necessity and possible contracting for claims to pay correctly.
- If there is no prior authorization in place, the claim will be denied, and the member could be charged.
See Out-of-Area/Out-of-State Spouse or Dependents for additional information. - Prior authorization is NOT required for urgent or emergency care – which are covered anywhere in the continental U.S.
Provider Tips by Type of Care
ABA therapy is an approach that uses positive reinforcement to improve behaviors and social interactions and decrease inappropriate behaviors. Education of the member and their caregivers is completed to reinforce positive behaviors in an effort to help the member accomplish activities of daily living (ADL’s).
ABA Benefits by Plan
- Medicaid
- ABA benefits are managed exclusively by the State of Colorado. Submit prior authorization requests directly to the State.
- ABA benefits are managed exclusively by the State of Colorado. Submit prior authorization requests directly to the State.
- Children Health Plan Plus (CHP+)
- ABA is not a covered benefit for DHMP or the State for CHP+ members.
- ABA is not a covered benefit for DHMP or the State for CHP+ members.
- DHHA | Exchange/CO Option
- ABA is managed by Denver Health Medical Plan (DHMP)
- DHMP requires authorization for ABA therapy services. ABA therapy is allowed for Exchange/CO Option and DHHA plans, with a confirmed diagnosis of autism.
Behavioral Health is defined as the treatment of mental and substance use disorders and the support of those who experience and/or are in recovery from these conditions, along with their families and communities.
Behavioral Health Benefits by Plan
- Medicare | Exchange/CO Option | DHHA | Children Health Plan Plus (CHP+)
- Managed by Denver Health Medical Plan (DHMP)
- DHMP requires prior authorization for some behavioral health services. Outpatient behavioral health therapy (individual or group) does not require prior authorization when provided in network. Please refer to the appropriate member handbook for benefits and exclusions.
- Managed by Denver Health Medical Plan (DHMP)
- Medicaid
- Colorado Access (COA)
- COA manages the behavioral health (BH) capitated program for DHMP members. Benefits are held exclusively by COA for review and subsequent approval or denial. DHMP does not have authority over the capitated BH benefits or any wrap around BH benefits administered by Health First Colorado (fee-for-service); therefore, DHMP cannot issue an approval or denial for those services.
- Effective 7/1/2025 DHMP is no longer responsible for any of the Short-Term Behavioral Health (STBH) Benefit codes.
- These codes are now included in the Behavioral Health Capitation program and are covered by the Regional Accountable Entity (RAE) Colorado Access (COA). The standard psychotherapy services that were billable under the STBH Benefit will continue to be covered by Medicaid when provided in a Primary Care Medical Provider (PCMP) setting; however, these services must be billed to the RAE effective 7/1/2025.
- CPT Codes
90791 - Diagnostic Evaluation without Medical Services
90832 - Psychotherapy-30 minutes
90834 - Psychotherapy-45 minutes
90837 - Psychotherapy-60 minutes
90846 - Family Psychotherapy (w/o patient)
90847 - Family Psychotherapy (with patient) - Colorado Access Prior Authorization of Services
- COA manages the behavioral health (BH) capitated program for DHMP members. Benefits are held exclusively by COA for review and subsequent approval or denial. DHMP does not have authority over the capitated BH benefits or any wrap around BH benefits administered by Health First Colorado (fee-for-service); therefore, DHMP cannot issue an approval or denial for those services.
- Elevate Medicaid Choice (DHMP)
- DHMP is responsible for a subset for Behavioral Health related services and supports.
- Colorado Access (COA)
Please see Breast Pumps for mothers of newborns for information on how to order breast pumps.
Breast pumps may be limited to the standard equipment provided by a DME provider contracted with DHMP. To receive a breast pump:
- The member must be at or beyond 28 weeks of pregnancy.
- The member’s doctor must submit a breast pump order directly to vendor.
- The member can pick up their breast pump or have it shipped directly to them.
Breast Pump Coverage by Plan
- DHHA | Exchange/CO Option
- A fully covered standard breast pump can be ordered through DHMP’s preferred vendors without prior authorization.
- The breast pump allowance is $150 per pregnancy and will cover a standard model If the member selects a breast pump with a higher value than the allowance, then the member will pay the price difference directly to the vendor.
- Medicaid | Medicare | Child Health Plan Plus (CHP+)
- Both manual (CPT Code E0602) and double-electric (CPT Code E0603) breastfeeding pumps are a covered benefit. If the member selects a breast pump with a higher value than the allowance, then the member will pay the price difference directly to the vendor.
- Prior authorization is not required when:
- Ordered through our *Preferred Vendors
- Breast pump is under $500
- Purchased (NU) modifier
- A prior authorization is required when:
- Vendor is not a *Preferred Vendor
- Breast pump is over $500
- Rented (RR) modifier
Contact Us
If you have a question regarding member benefits, please call Health Plan Services at 303-602-2100 or toll-free at 1-800-700-8140. If you need assistance finding vendors or coordinating care, please call Care Management at 303-602-2184 or email us at DHMPMaternalCare@dhha.org.
What is a Cochlear Implant?
A cochlear implant is a small, complex electronic device that can help to provide a sense of sound to a person who is profoundly deaf or severely hard-of-hearing. An implant consists of an external portion that sits behind the ear and a second portion that is surgically placed under the skin. An implant has the following parts:
- A microphone, which picks up sound from the environment
- A speech processor, which selects and arranges sounds picked up by the microphone
- A transmitter and receiver/stimulator, which receive signals from the speech processor and convert them into electric impulses
- An electrode array, which is a group of electrodes that collects the impulses from the stimulator and sends them to different regions of the auditory nerve
An implant does not restore normal hearing. Instead, it can give a deaf person a useful representation of sounds in the environment and help him or her to understand speech. A cochlear implant is very different from a hearing aid. Hearing aids amplify sounds, so they may be detected by damaged ears. Cochlear implants bypass damaged portions of the ear and directly stimulate the auditory nerve. Children and adults who are deaf or severely hard-of-hearing can be fitted for cochlear implants or other cochlear devices. Below are the DHMP benefits by plan for cochlear implants, including the entity that is responsible for review and management of services.
Cochlear Implant Benefits by Plan
- Medicaid
- Managed by State of Colorado
Benefits are administered exclusively by the State of Colorado for review and subsequent approval or denial. Submit prior authorization requests to the State of Colorado. Refer to the fee schedule for coverage and pricing.
- Managed by State of Colorado
- Exchange/CO Option | DHHA | Medicare | Child Health Plan Plus (CHP+)
- Managed by DHMP
Cochlear implants or other cochlear devices are a covered benefit with prior authorization, upon determination of medical necessity. Inpatient and outpatient charges apply. Member handbooks provide additional details and can be found on each plan member page, under the 'Members' tab of this website.
- Managed by DHMP
Colorado’s Early Intervention program provides support and services to children with developmental delays or disabilities and their families from birth until the child’s third birthday.
EIS by Plan
- Exchange/CO Option | DHHA | Child Health Plan Plus (CHP+)
- Members are managed via the Trust Fund -- only HIA and IFSP forms are to be submitted
- Members are managed via the Trust Fund -- only HIA and IFSP forms are to be submitted
- Medicaid
- Medicaid members require prior authorization for all EIS care
- Initial Authorization Requests
- 30-day retroactive reviews are allowed for initial evaluations ONLY for PT/ST/OT
- Current IFSP is required for initial start of services
- Continued Care or Extension of Services
- Any modification (extended dates or additional visits) requires a new submission
- A current IFSP is required for continued or extension of services
- Summary document or current clinical with progression/regression and functional status from Therapist are needed for each new request
The designation of homebound is contingent upon a patient’s individual ability – not caregiver support.
Home Health Care Qualifications by Plan
- Medicare
- CMS defines 'homebound' as normally unable to leave home unassisted. To be homebound means that leaving home takes considerable and taxing effort. A person may leave home for medical treatment or short, infrequent absences for non-medical reasons, such as a trip to the barber or to attend religious service. Due to illness or injury, member needs the aid of supportive devices such as crutches, canes, wheelchairs, walkers, special transportation or the help of another person to leave their place of residence.
- Member must be under the care of a doctor who must have a plan of care for that she or he regularly reviews.
- The in-home health agency must be Medicare-approved.
- Member's doctor must certify that they are unable to leave home without some difficulty – for example, member might need transportation and/or help from a cane, walker, wheelchair and/or someone to help them. In other words, member is homebound.
- CMS defines 'homebound' as normally unable to leave home unassisted. To be homebound means that leaving home takes considerable and taxing effort. A person may leave home for medical treatment or short, infrequent absences for non-medical reasons, such as a trip to the barber or to attend religious service. Due to illness or injury, member needs the aid of supportive devices such as crutches, canes, wheelchairs, walkers, special transportation or the help of another person to leave their place of residence.
- Exchange/CO Option | DHHA
- Medical Conditions/Acute Illness or Injury
- A patient will be considered to be homebound if they have a condition, due to an illness or injury, which restricts their ability to leave their place of residence except with the aid of supportive devices such as crutches, canes, wheelchairs and walkers.
- Absences from the home must be infrequent, of short duration and usually to receive medical care not available at home, e.g., hemodialysis or chemotherapy.
- Psychiatric Conditions or Developmental Delay
- Psychiatric patients can have a homebound status if illness manifests into refusal to leave the home or if not leaving the home will lessen ability to obtain full benefits of therapy outside the home (such as but not limited to severe depression, paranoia, agoraphobia, anxiety).
- Homebound applies for students with disabilities who are unable to attend school.
- Clinical Judgement
- On rare occasions there may extenuating circumstances that justify the need for services in the home. These types of cases should be reviewed on a case-by-case bases and by the Medical Director for determination.
- Members should be referred for Case Management assistance if not already in a Case Management Program.
- Medical Conditions/Acute Illness or Injury
- Medicaid
- There are two types of HHC services:
- Acute HHC home health services are provided to members who experience an acute health care need that requires skilled services such as: skilled nursing, skilled certified nurse aide, physical therapy, occupational therapy, speech therapy and telehealth services.
Acute HHC services are allowed up to 60 calendar days or until the acute condition is resolved, whichever comes first. - Long Term HHC goes beyond 60 days, is a wrap benefit and requests must be prior authorized with the state.
- Acute HHC home health services are provided to members who experience an acute health care need that requires skilled services such as: skilled nursing, skilled certified nurse aide, physical therapy, occupational therapy, speech therapy and telehealth services.
- If a member experiences a new acute event that would warrant Acute HHC service, the agency may move the member to acute care, when:
- At least ten (10) calendar days has elapsed since the member's last Acute HHC episode, and
- There is new onset of illness, injury, or disability or when the member experiences an acute change in condition from the member's past acute HHC episode(s).
- Health First Colorado Members qualify who:
- Require HHC services for the treatment or management of an illness, injury, or disability, which may include mental illness (acute).
- Are unable to perform the health care tasks for him or herself, and he or she has no family member/caregiver who is willing and able to perform the skilled tasks.
- Require services that cannot appropriately or effectively be received in an outpatient treatment office or clinic or for which the member's residence is the most effective setting to accomplish the care required by the member's medical condition (clinical judgement).
- The services meet medical necessity criteria and are provided in a manner consistent with professional practice.
- Refer to: Colorado Department of Health Care Policy & Financing | Home Health Program
- There are two types of HHC services:
- Child Health Plan Plus (CHP+)
- Covered services include:
- Skilled nursing care provided on a defined schedule
- Physical, occupational, and respiratory therapy
- Administration of oxygen
- Intravenous medications and other prescription drugs ordinarily not available through a retail pharmacy
- Physician home visits
- Not covered:
- Custodial care
- Care provided by a nurse who lives in the patient’s home
- Food or meal services other than dietary counseling
- Care related to noncovered services
- Personal comfort of convenience items or services
- Care provided in a skilled nursing facility
- There is no EIS therapy benefit for developmental delays after the 3rd birthday for CHP+ Members
- HHC is available for our members for short durations to help resolve an acute illness or injury
- ABA is not a covered benefit for DHMP or the state for CHP+ members
- Covered services include:
Infertility Coverage by Plan
- Exchange/CO Option | DHHA
- Infertility is a covered benefit for only Exchange/CO Option and DHHA plans. Please reference the specific member handbook linked below for benefit details, limitations, and exclusions.
Infertility Definitions
- Infertility - Failure to conceive following 1 or more of the following:
- At least 1 year of regular unprotected sexual intercourse for female age 35 years or younger
- At least 6 months of regular unprotected sexual intercourse for female older than 35 years
- Failure to Impregnate or Conceive - The failure to establish a clinical pregnancy after twelve months of regular, unprotected sexual intercourse or therapeutic donor insemination for a woman under the age of thirty-five, or after six months of regular, unprotected sexual intercourse or therapeutic donor insemination for a woman thirty-five years of age or older. Conception resulting in a miscarriage does not restart the twelve-month or six-month clock to qualify as having infertility.
- Iatrogenic Infertility - An impairment of fertility by surgery, radiation, chemotherapy, or other medical treatment affecting reproductive organs or processes.
- Diagnosis of and Treatment for Infertility - The procedures and medications recommended by a licensed physician that are consistent with established, published, or approved medical practices or professional guidelines from ACOG or ASRM for diagnosing and treating infertility.
- Preimplantation Genetic Testing (PGT) - A test performed to analyze the DNA from oocytes or embryos for human leukocyte antigen (HLA)-typing or for determining genetic abnormalities. These include:
- PGT-A: For aneuploidy screening (formerly PGS)
- PGT-M: For monogenic/single gene defects (formerly single-gene PGD)
- PGT-SR: For chromosomal structural rearrangements (formerly chromosomal PGD) (Zegers-Hochschild et al., 2017)
- Therapeutic Donor Insemination (TDI) - Insemination with a donor sperm sample for the purpose of conceiving a child. The donor can be an anonymous or directed donor.
To Submit a Prior Authorization Request
- All services for infertility require prior authorization, including office visits. See Services Requiring Prior Authorization for a full list of services that require prior authorization.
- Complete a Prior Authorization Request form and submit it to DHMP Utilization Management, along with clinical records supporting medical necessity. You can submit through the DHMP Provider Portal or by fax.
- To Submit through the Provider Portal
Create a Provider Portal account under 'Register Here'' (see Provider Portal Guide for instructions). Complete the Prior Authorization Request Form, attach clinicals and submit. - To Submit by Fax
Send Prior Authorization Request form and clinicals.
– Outpatient fax: 303-602-2128
– Inpatient Admit and Discharge Notification fax: 303-602-2127
– Inpatient Clinical Records fax: 303-602-2004
– Urgent/Expedited fax: 303-602-2160
- To Submit through the Provider Portal
Reference Materials
DHHA Member Handbooks (EOCs)
DHHA Employer Plans Pharmacy
Elevate Exchange/CO Option Member Handbooks (EOCs)
Elevate Exchange/CO Option Pharmacy
Neuropsychological tests are specifically designed tasks that are used to measure a psychological function, known to be linked to a brain structure or pathway. Tests are used for research into brain function and in a clinical setting, for the diagnosis of deficits.
Medicaid Neuropsychology Testing Benefits
Managed by Colorado Access (Behavioral Health Diagnosis).
For neuropsychology testing, there is a procedure code component and a diagnostic component for services included in the behavioral health benefit. Neuropsychology testing is covered by the capitated behavioral health program which is managed by Colorado Access (COA). If neuropsychology testing is for a behavioral health diagnosis, please fax requests, using the Medicaid Psychological Testing Prior Authorization Form to 720-744-5130. The list of procedure codes is found on page two of the form.
Newborn Assignment and Process
- Newborn Plan Attribution
A Newborn's plan attribution is based on the mother/oldest female on the case eligibility and plan assignment. The newborn will be attributed to the same plan (e.g., RAE or MCO). Newborns should not be attributed to DHMP until:- They have received their own Medicaid ID; and
- They have been discharged from the hospital
- NICU/Extended Inpatient Stay
If a baby is born and goes directly to NICU or requires an extended inpatient stay at time of birth:- Once the newborn is assigned a Medicaid ID, the State/HCPF will attribute the newborn to DHMP if the mother lives in Denver County. Unfortunately, the State cannot know if a newborn is still inpatient after being born.
- When this occurs, DHMP can request a disenrollment for the newborn based on the inpatient stay rules that do not allow a member to change their plan attribution during an inpatient stay.
- Newborn Medicaid ID
Newborns who do not have a Medicaid ID assignment cannot be verified in the Provider Portal. If you provide services and the newborn is enrolled with DHMP:- Submit an authorization request to the Utilization Management team for review.
- The guardian of the newborn has 90 days after the date of enrollment into DHMP to transition services into the Denver Health system or to disenroll from DHMP.
- DHMP will review and authorize services for the newborn during the time of assignment to the Plan.
- The mother/guardian must contact Health First Colorado to request a disenrollment from DHMP.
- After 90 days, if the member does not contact Health First Colorado and request a disenrollment, the newborn will be locked into DHMP until their open enrollment period and will need to obtain services through the Denver Health system.
For Additional Information
Member Contacts
Colorado Medical Assistance Program (CMAP)
For assistance with updating demographics, income, adding/removing members
1-800-221-3943
DHMP Health Plan Services
303-602-2116
Health First Colorado Enrollment
To request plan change within initial 90 Days
303-839-2120
Health First Colorado
For general questions about Health First Colorado
1-800-221-3943
Provider Contacts
DHMP Health Plan Services
For member enrollment/eligibility questions
303-602-2100
Learn more about the DHMP Medicaid Attribution process.
The following is intended to provide guidance to providers regarding outpatient therapy services and benefit limitations by plan. Please be aware that physical therapy, occupational therapy, and speech therapy will be authorized only until maximum medical improvement is reached or annual benefit is exhausted, whichever comes first.
Outpatient Therapy Definitions
- Acute Condition - Acute injuries/conditions/diseases come on rapidly and are accompanied by distinct symptoms that require urgent or short-term care and get better once they are treated.
- Chronic Condition - A chronic condition, disease, or developmental delay that persists over a prolonged period of time and is long lasting in its effects.
- Developmental Delay - Refers to a child who has not gained the developmental skills expected compared to others of the same age. Delays may occur in the areas of motor function, speech, and language, cognitive, play, and social skills. Global developmental delay means a young child has significant delays in two or more of these areas of development.
- Discharge From Care - If the member fails to participate, is no longer progressing, meeting goals or has plateaued in their therapy, the member is to be discharged from therapy.
- Outpatient Therapy - Course of treatment(s) to support members recovery and rehabilitation, delivered through a series of visits at a therapy practice or a clinic.
- Habilitative Services - Services that help a person DEVELOP skills or functions they didn't have before and to help a person keep, learn, or improve skills and functioning for daily living with a chronic disease, condition or developmental delay.
- Rehabilitative Services - Help a person GET BACK or IMPROVE skills and functioning for daily living that have been lost or impaired because of an acute occurrence such as sudden illness and/or injury. The therapy is aimed at improving, adapting, or restoring functions which have been impaired or permanently lost because of illness, injury, loss of a body part, or congenital abnormality.
- Occupational Therapy - Improves ability to take part in everyday activities to complete fine motor skills for activities of daily living (i.e., feeding, grooming). Occupational therapists address functioning everyday environment and can work in tandem with Speech therapy for swallowing studies and food aversion type issues.
- Physical Therapy - Restores, improves, or maintains movement and function. Use of targeted exercises and other treatments to help restore, improve, or maintain range of motion and gross motor ability. Provided by physical therapists who optimize the quality of life through prescribed exercise, hands-on care, and patient education.
- Speech Therapy - Improves ability to generate words, use language and 2-way communication. Speech therapists will be able to support in key areas related to speech (verbal communication), language (processing communication), cognitive functioning (processing and use of information) in tasks that involve memory, holding attention, and problem-solving).
Outpatient Therapy (PT, OT, ST) Prior Authorization Requirements
- Participating Network Providers (Tier 1 Providers):
- Rehabilitative: No authorization for first 30 visits
- Habilitative: No authorization for first 30 visits
- Authorization required for visit 31 forward and must meet medical necessity criteria
- Non-Participating Out-of-Network Providers (Tier 2 and 3 Providers):
- Require authorization (prior to services being rendered) on day 1 of therapy services (rehabilitative and habilitative).
- All care must meet medical necessity criteria and be a benefit.
Outpatient Therapy Benefits and Limitations by Plan
Physical therapy, occupational therapy and speech therapy will be authorized only until maximum medical improvement is reached or annual benefit is exhausted, whichever comes first. There are no limits for speech therapy to treat cleft lip or cleft palate (applies for all lines of business).
- Medicare | Medicaid
- No benefit limit, but all requests must meet medical necessity per regulatory guidelines (rehabilitative & habilitative)
- No benefit limit, but all requests must meet medical necessity per regulatory guidelines (rehabilitative & habilitative)
- Exchange/CO Option | DHHA
- Thirty visit limit per calendar year per diagnosis, additional services may be provided with a prior authorization if deemed medically necessary
- Thirty visit limit per calendar year per diagnosis, additional services may be provided with a prior authorization if deemed medically necessary
- Child Health Plan Plus (CHP+)
- Thirty visit limit per calendar year per diagnosis, additional services may be provided with a prior authorization if deemed medically necessary
- Habilitative/Maintenance care is not covered
- Services must be received within six months from the date the injury or illness occurred
- There is no limit for therapies for children from birth up to the child’s third birthday
- There is no benefit for any therapy for developmental delays after the third birthday
Reference Documents
Find provider documents and reference materials in the resource library.

