Provider Participation Status Definitions
Provider Participation Status is identified and described as follows:
- Tier 1 Providers** - Contracted providers considered in-network, listed in the Provider Directory and do not require authorization unless service is included in the AUTHORIZATION CATEGORIES below (excludes DHHA).
- Tier 2 Providers** - Contracted Providers considered out-of-network, not listed in the Provider Directory, and require prior authorization for all services.
- Tier 3 Providers** - Non-contracted, out of network providers for all lines of business, not listed in the Provider Directory, require prior authorization for all services and may require a One Time Agreement (OTA).
**Provider tiering status may vary by line of business.
**Services must meet medical necessity and be a covered benefit, regardless of provider tiering status.
General Rules
- Urgent and Emergency Care DO NOT require Prior Authorization.
- DHHA facilities and DHHA providers who perform services at DHHA do not require prior authorization for any services.
- Services not requiring prior authorization are subject to audit. If in an audit, services did not meet medical necessity, there will be a possibility of recoupment.
- Excluded services are not covered. Excluded services will be denied as a non–covered benefit, per the member’s Evidence of Coverage (EOC).
- Providers are responsible for verifying eligibility and benefits before providing services to all DHMP members. Prior Authorization is not a guarantee of payment for services. Payment is made in accordance with a determination of the member’s eligibility, benefit limitations/exclusions, evidence of medical necessity during the claim review and provider status with DHMP.
- Failure to obtain prior authorization before providing care for the services listed below may result in a denial for reimbursement.
- If a DHMP member is admitted to your facility, you must notify DHMP within 24 hours. If you fail to notify DHMP during this window of time, the member’s admission and continued stay may be denied for “untimely notification.”
Resources
Providers can submit Prior Authorization Requests by either submitting an ONLINE Prior Authorization Request form or by completing and faxing a PDF Prior Authorization Request form. If using a PDF form, it should be faxed to DHMP. If you have questions, please contact Health Plan Services at 303-602-2100.
- Inpatient Request Fax: 303-602-2127
- Outpatient Request Fax: 303-602-2128
- Urgent/Expedited Request Fax: 303-602-2160
UM PRIOR AUTHORIZATION REQUEST FORM
Denver Health Medical Plan Secondary Payer and Authorizations
Denver Health Medical Plan (DHMP) does not typically require authorization when the secondary payer. However, if the requested service was denied by the primary insurance as not a covered benefit or benefits have been exhausted, an authorization may be requested.
Please submit clinical information with the primary insurances denial letter or limitation/exhaustion letter with the authorization request to the Utilization Management (UM) Department.
Note: Prior Authorization is not a guarantee of payment for services. Payment is made in accordance with a determination of the member’s eligibility, benefit limitations/exclusions, and evidence of medical necessity during the authorization review and provider status with DHMP at the time services are rendered.
Denver Health Medical Plan Secondary Payer and Claims
Submit claims to the secondary insurance once you have billed the primary insurance and received payment or Explanation of Remittance (EOR). DHMP will need the bill total, how much the primary insurance paid and why primary didn’t pay the remainder of the balance.
Please include the adjustments and categories for the remaining balance for a seamless secondary claim process.
Secondary coverage may only cover part or all the remaining costs or not pay any of the remaining costs. There are steps in place to ensure that both plan/coverages do not pay more than 100% of the bill based on contractual and benefit plan arrangements.
Provider Forms and Materials
Providers refer to the PROVIDER FORMS AND MATERIALS page for provider forms, as well as provider tips for general guidance, information on select services and internal clinical coverage criteria.
Authorization Categories
| Care Type | Details |
|---|---|
| Acute Physical Rehabilitation | All acute/inpatient requires prior authorization |
| Any Experimental/Investigational Services | Experimental/Investigational medical and surgical procedures, equipment, and medications |
| Behavioral Health Services |
(Medicare Tier 1 Providers do not require authorization for any Behavioral Health Services) |
| Durable Medical Equipment (DME) and Prosthetics | All DME and Prosthetics with a purchase price of $500 or greater (Billed with modifier NU or UE) (Limitations and/or requirements may apply) |
| Durable Medical Equipment (DME) Rental | All DME Rentals regardless of dollar amount (billed with modifier RR) (Limitations and/or requirements may apply) |
| Disposable goods | Authorization required if beyond benefit limit (Limitations and/or requirements may apply) |
| Early Intervention Services | Medicaid: PT, OT and ST under 3 years of age CHP+, DHHA and Exchange/CO Option: Members are managed via the Trust Fund -- only HIA and IFSP forms are to be submitted |
| Enteral and Total Parenteral Nutrition | All oral, tube feed or TPN requires prior authorization |
| Genetic Testing |
Tier 2 and Tier 3 Non-Participating (Out of Network) Providers require authorization for all genetic testing. |
| Home Health |
|
| Infertility Treatment | All infertility treatment services related to the inability to achieve pregnancy |
| Outpatient Physical Therapy (PT), Occupational Therapy (OT) and Speech Therapy (ST) | Tier 1 Providers
|
| The following surgeries when performed in an inpatient, outpatient or office location |
Providers are responsible for verifying eligibility and benefits before providing services to all DHMP members |
| Long Term Acute Care (LTAC) |
|
| Skilled Nursing Facility (SNF) |
|
| Some Specialty Rx/Infusions (Based on Federal and State regulatory guidelines and/or benefit plan limitations) | See list at the end of this document |
| Transplants |
|
*Based on Federal and State regulatory guidelines and/or benefit plan limitations. Exclusion, limitations and/or requirements may apply.
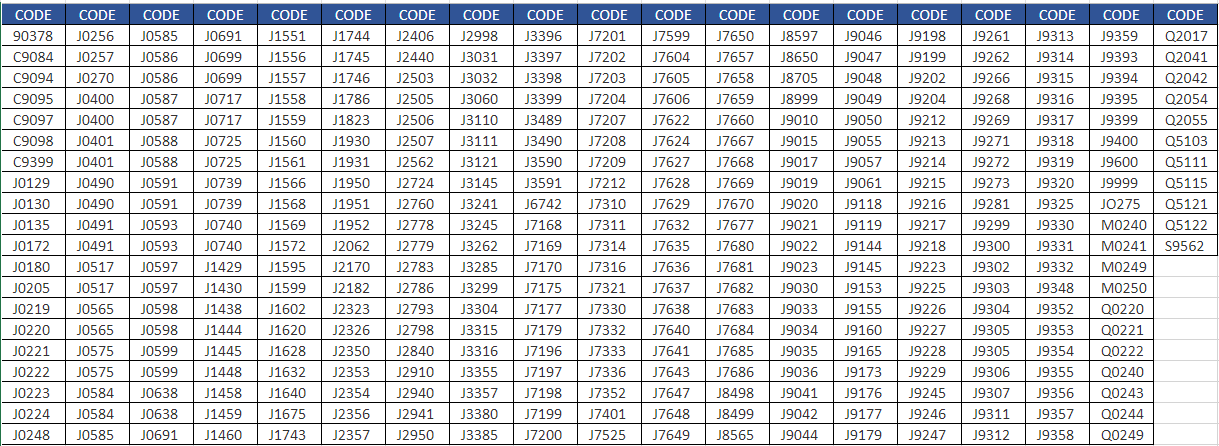
Specialty Rx/Infusions Requiring Prior Authorization
If you have questions, please contact Health Plan Services at 303-602-2100.

